What Causes Pain In The Heel And Approaches To Deal With It
Overview
Plantar fasciitis is an inflammation of the structures (of the plantar fascia) on the sole of the foot. The inflammation is caused by excess pressure on the structures on the sole of the foot. The plantar fascia becomes inflamed and tiny rips can occur where it attaches into the inside of the heel bone. It tends to be most painful first thing in the morning, or when standing up after sitting for a while. The area becomes inflamed and swollen, and it is the increase in fluid to the area that accumulates when weight is taken off the area, that then causes the pain on standing. Plantar Fasciitis usually starts gradually with pain on standing after rest. Pain is usually located under the heel or to the inside of the heel. Pain is usually at its worst on standing first thing in the morning. The pain will begin to ease once you get moving. Pain in the early stages tends to occur after activity rather than during activity. As plantar fasciitis continues the pain can become more constant and can then start to affect the way you walk.
Causes
Plantar fasciitis occurs when the thick band of tissue on the bottom of the foot is overstretched or overused. This can be painful and make walking more difficult. You are more likely to get plantar fasciitis if you Have foot arch problems (both flat feet and high arches), run long distances, downhill or on uneven surfaces, are obese or gain weight suddenly, have a tight Achilles tendon (the tendon connecting the calf muscles to the heel), wear shoes with poor arch support or soft soles. Plantar fasciitis is seen in both men and women. However, it most often affects active men ages 40 - 70. It is one of the most common orthopedic foot complaints. Plantar fasciitis was commonly thought to be caused by a heel spur. However, research has found that this is not the case. On x-ray, heel spurs are seen in people with and without plantar fasciitis.
Symptoms
Plantar fasciitis typically causes a stabbing pain in the bottom of your foot near the heel. The pain is usually worst with the first few steps after awakening, although it can also be triggered by long periods of standing or getting up from a seated position.
Diagnosis
Diagnosis of plantar fasciitis is based on a medical history, the nature of symptoms, and the presence of localised tenderness in the heel. X-rays may be recommended to rule out other causes for the symptoms, such as bone fracture and to check for evidence of heel spurs. Blood tests may also be recommended.
Non Surgical Treatment
Treatment for plantar fasciitis should begin with rest, icing, and over the counter medications. As mentioned above, an orthotic is a device that can be slipped into any pair of shoes and can often relieve pain and help to reverse the damage and occurrence of plantar fasciitis. They do this by adding support to the heel and helping to distribute weight during movement. In addition to orthotics, many people consider night splints for treating this condition. These devices are worn during the night while you sleep, helping to keep the plantar fascia stretched to promote healing. Physical therapy has also become a common option. With this conservative treatment alternative, a physical therapist designs a set of exercises that are intended to address your specific needs in order to promote healing.

Surgical Treatment
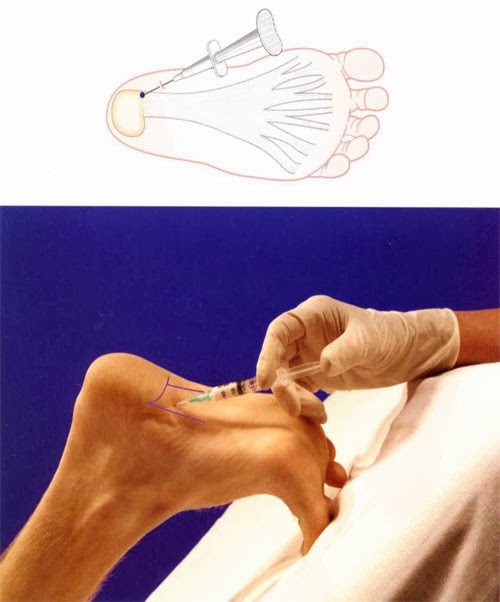
Surgery is rarely needed in the treatment of plantar fasciitis. The vast majority of patients diagnosed with plantar fasciitis will recover given ample time. With some basic treatment steps, well over 90% of patients will achieve full recovery from symptoms of plantar fasciitis within one year of the onset of treatment. Simple treatments include anti-inflammatory medication, shoe inserts, and stretching exercises. In patients where a good effort with these treatments fails to provide adequate relief, some more aggressive treatments may be attempted. These include cortisone injections or extracorporeal shock wave treatments.
Stretching Exercises
In one exercise, you lean forward against a wall with one knee straight and heel on the ground. Your other knee is bent. Your heel cord and foot arch stretch as you lean. Hold for 10 seconds, relax and straighten up. Repeat 20 times for each sore heel. It is important to keep the knee fully extended on the side being stretched. In another exercise, you lean forward onto a countertop, spreading your feet apart with one foot in front of the other. Flex your knees and squat down, keeping your heels on the ground as long as possible. Your heel cords and foot arches will stretch as the heels come up in the stretch. Hold for 10 seconds, relax and straighten up. Repeat 20 times. About 90 percent of people with plantar fasciitis improve significantly after two months of initial treatment. You may be advised to use shoes with shock-absorbing soles or fitted with an off-the-shelf shoe insert device like a rubber heel pad. Your foot may be taped into a specific position. If your plantar fasciitis continues after a few months of conservative treatment, your doctor may inject your heel with steroidal anti-inflammatory medication. If you still have symptoms, you may need to wear a walking cast for two to three weeks or a positional splint when you sleep. In a few cases, surgery is needed for chronically contracted tissue.
What Triggers Heel Pain And Ways To Heal It

Overview
Plantar fasciitis is a condition that causes heel and arch pain through inflammation on the bottom of the foot. The part that’s inflamed (swollen) is actually the plantar fascia, which is the connective tissue or ligament that stretches from the base of the toes, across the arch of the foot, and inserts into the heel bone. This painful condition can interfere with your daily activity and severely decrease your quality of life.
Causes
When some people stand/walk/run/jump their own anatomy in their ankle joint is not ‘sturdy’ enough to cope with the needed stabilisation of their ankle joint when they are weight bearing. So, their ankle rotates to find a point of stability. By the shin twisting in and the ankle rotating downwards to the inside (along with your body weight, the power of some muscles, and of course, gravity) a huge amount of stress is applied to the plantar fascia until it is stressed beyond it’s normal limits and it starts to ‘tighten up’. It is this tightening up of the plantar fascia under this stress that causes the damage that in turn leads to pain…eventually.
Symptoms
When plantar fasciitis occurs, the pain is typically sharp and usually unilateral (70% of cases).Heel pain worsens by bearing weight on the heel after long periods of rest. Individuals with plantar fasciitis often report their symptoms are most intense during their first steps after getting out of bed or after prolonged periods of sitting. Improvement of symptoms is usually seen with continued walking. Numbness, tingling, swelling, or radiating pain are rare but reported symptoms. If the plantar fascia continues to be overused in the setting of plantar fasciitis, the plantar fascia can rupture. Typical signs and symptoms of plantar fascia rupture include a clicking or snapping sound, significant local swelling, and acute pain in the sole of the foot.
Diagnosis
Your doctor will check your feet and watch you stand and walk. He or she will also ask questions about your past health, including what illnesses or injuries you have had. Your symptoms, such as where the pain is and what time of day your foot hurts most. How active you are and what types of physical activity you do. Your doctor may take an X-ray of your foot if he or she suspects a problem with the bones of your foot, such as a stress fracture.
Non Surgical Treatment
Most health care providers agree that initial treatment for plantar fasciitis should be quite conservative. You'll probably be advised to avoid any exercise that is making your pain worse. Your doctor may also advise one or more of these treatment options. A heel pad. In plantar fasciitis, a heel pad is sometimes used to cushion the painful heel if you spend a great deal of time on your feet on hard surfaces. Also, over-the-counter or custom-made orthotics, which fit inside your shoes, may be constructed to address specific imbalances you may have with foot placement or gait. Stretching: Stretching exercises performed three to five times a day can help elongate the heel cord. Ice: You may be advised to apply ice packs to your heel or to use an ice block to massage the plantar fascia before going to bed each night. Pain relievers: Simple over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, are often helpful in decreasing inflammation and pain. If you have stomach trouble from such drugs, your health care provider may prescribe an alternative. A night splint: A night splint is sometimes used to hold your foot at a specific angle, which prevents the plantar fascia from shortening during sleep. Ultrasound: Ultrasound therapy can be performed to decrease inflammation and aid healing. Steroid injections: Anti-inflammatory steroid injections directly into the tissue around your heel may be temporarily helpful. However, if these injections are used too many times, you may suffer other complications, such as shrinking of the fat pad of your heel, which you need for insulation. Loss of the fat pad could actually increase your pain, or could even rupture the plantar fascia in rare cases. Walking cast: In cases of long-term plantar fasciitis unresponsive to usual treatments, your doctor may recommend that you wear a short walking cast for about three weeks. This ensures that your foot is held in a position that allows the plantar fascia to heal in a stretched, rather than shortened, position. Shock wave therapy, Extracorporeal shock wave therapy which may be prescribed prior to considering surgery if your symptoms have persisted for more than six months. This treatment does not involve any actual incisions being made rather it uses a high intensity shock wave to stimulate healing of the plantar fascia.

Surgical Treatment
Plantar fasciotomy is often considered after conservative treatment has failed to resolve the issue after six months and is viewed as a last resort. Minimally invasive and endoscopic approaches to plantar fasciotomy exist but require a specialist who is familiar with certain equipment. Heel spur removal during plantar fasciotomy has not been found to improve the surgical outcome. Plantar heel pain may occur for multiple reasons and release of the lateral plantar nerve branch may be performed alongside the plantar fasciotomy in select cases. Possible complications of plantar fasciotomy include nerve injury, instability of the medial longitudinal arch of the foot, fracture of the calcaneus, prolonged recovery time, infection, rupture of the plantar fascia, and failure to improve the pain. Coblation (TOPAZ) surgery has recently been proposed as alternative surgical approaches for the treatment of recalcitrant plantar fasciitis.
Exercise Routines For Heel Pain and Heel Spur Treatment Options
If changing your shoes isn't helping to solve your foot pain, it is time for us to step in. Contact Dr. Jeff Bowman at Houston Foot Specialists for treatment that will keep your feet feeling great. Inserting arch support insoles in the shoes is also a good option.
Those affected by inflammatory conditions such as rheumatoid arthritis and Achilles tendonitis are also likely to experience pain and swelling in the ankles. If the joints in the feet get affected by osteoarthritis, it gives rise to pain, stiffness, swelling in or around the joint, and restricted range of motion. Since pain in the feet could be caused due to a variety of reasons, the treatment will depend on the underlying cause. Many a time, pain could be experienced by people who perform high-impact exercises such as running, jogging and other sports. Those who have been experiencing pain while running must make sure that they wear a good quality footwear. Painkillers or steroids might be prescribed for the treatment of a sprained ankle.

The spur occurs where the plantar fascia attaches, and the pain in that area is really due to the plantar fascia attachment being irritated. However, there are many people with heel spurs who have no symptoms at all. Haglund's deformity is a bony growth on the back of the heel bone, which then irritates the bursa and the skin lying behind the heel bone. Achilles tendinopathy is degeneration of the tendon that connects your calf muscles to your heel bone. Stress fractures are common in military training.
Junctional Epidermolysis Bullosa: A condition that causes blistering of the skin because of a mutation of a gene which in normal conditions helps in the formation of thread-like fibers that are anchoring filaments, which fix the epidermis to the basement membrane. Kanner Syndrome: Also referred to as Autism, this is one of the neuropsychiatric conditions typified by deficiencies in communication and social interaction, and abnormally repetitive behavior. Kaposi's Sarcoma: A kind of malignancy of the skin that usually afflicts the elderly, or those who have problems in their immune system, like AIDS. For example, a year of perfect health is regarded as equivalent to 1.0 QALY.
Pictures, Remedies & Treatment
Hand, foot and mouth disease is usually spread from person- to -person through faecal contamination (which can occur when changing a nappy or using the toilet and not properly washing hands afterwards), or spread through respiratory secretions (saliva, sputum, or nasal mucus) of an infected person. There is no clear evidence of risk to unborn babies from hand, foot and mouth disease. However, infected mothers can pass the infection onto newborn babies who rarely can have severe disease. Avoid sharing cups, eating utensils, items of personal hygiene (for example: towels, washers and toothbrushes), and clothing (especially shoes and socks). Children with hand, foot and mouth disease should be excluded from school or childcare facilities until their blisters have dried. Thus it helps loosen the hard and scaly skin.
There are four major stages with which pain will begin in our body. The first is the actual stimulus, which starts the pain information pathway to the brain. Before the electrical information finally enters the brain, the body has a third step in the pain route, called modulation. Once the brain accepts the electrical signal and final process begins, which is the awareness of pain in the body. The two main goals that a podiatrist wants to achieve in treating pain are to eliminate the source of the problem and also to treat the symptoms caused by the problem. In order to do so, the podiatrist will need to investigate the cause of the pain by first asking the patient a series of questions regarding the problem. There are different types of pain in the body. If the pain is tingling or burning, the problem is most probably associated with the nerve.
Most cases of foot pain can be treated without surgery, whether it's metatarsal foot pain, ball-of-foot pain, foot arch pain or some other type. At the start to notice soreness or discomforts around the foot area, it is imperative to take rest, put on or apply cold or ice compress, and or elevate the affected foot. Generally, foot pains vary from mild to severe. However, prevention is above all better than to deal with any pain though. Never take for granted to any pain; focus on getting foot pain reliever at the soonest is vital. In case the pain is unbearable which it hampers the usual life activities, it is imperative to look for urgent medical or therapist to help and also consider the ordinary methods to lessen foot pain. Stretching exercises also facilitate to soothe the muscles on the feet and help out in the contraction of the muscles. Not all skin disorders respond to treatment.
You might find some comfort in knowing that you are not the only one who has contracted toenail fungus; podiatrists estimate that six to eight percent of the population has onychomycosis, too. Topical creams: The ointments that you apply directly to the toenail aren't strong enough to combat this extraordinarily stubborn foot fungus.
Since plantar fascia gets tightened while one is asleep, the sudden movement causes stretching of the ligament as one takes the first few steps. While structural foot abnormalities such as high arches or fallen arches can make one more susceptible to plantar fasciitis, wearing old worn-out shoes can also cause stress to the plantar fascia. Those suffering from plantar fasciitis are also at an increased risk of developing heel spurs. Heel spurs, also known as osteophytes, are abnormal bony outgrowths that may develop along the edges of the heel bone. Heel spurs form when the plantar fascia starts pulling at the heel bone or gets torn due to excessive stress. If the heel spurs start impinging on any of the surrounding nerves or the tissues, one is likely to suffer from pain. Plantar fasciitis and heel spurs surely affect one's ability to move about freely. This is the best way to support the arch of the foot. Pain then sets in and you may need surgery.
Avoid sharing personal items like towels, footwear and clothes with other people. Podiatry is a branch of medicine that is focused on the study, diagnosis and ultimately, the treatment of disorders that occur on the foot, ankle or lower leg. Podiatrists are able to easily identify, diagnose and treat a foot related problem that a person is suffering from. You can also prevent foot problems by some exercising and stretching.

Achilles Tendonitis
 Achilles tendinitis is an overuse injury common in many sports that require lots of running and jumping. Once this condition becomes more chronic adhesions that form along the tissues and the injury becomes more of a tendinosis. Treatment for a tendinosis is much different that for a tendinitis, so it is important to recognize what stage the injury is at in order to treat it appropriately. An acute achilles tendinitis involves inflammation and would be treated with rest, ice, etc. Once the inflammation has decreased, research shows that eccentric exercises are beneficial. Once there is tendinosis, it becomes imperative to break up those adhesions with ART and prescribe appropriate stretches and exercises.
Achilles tendinitis is an overuse injury common in many sports that require lots of running and jumping. Once this condition becomes more chronic adhesions that form along the tissues and the injury becomes more of a tendinosis. Treatment for a tendinosis is much different that for a tendinitis, so it is important to recognize what stage the injury is at in order to treat it appropriately. An acute achilles tendinitis involves inflammation and would be treated with rest, ice, etc. Once the inflammation has decreased, research shows that eccentric exercises are beneficial. Once there is tendinosis, it becomes imperative to break up those adhesions with ART and prescribe appropriate stretches and exercises.
Causes
The majority of Achilles tendon injuries are due to overuse injuries. Other factors that lead to Achilles tendonitis are improper shoe selection, inadequate stretching prior to engaging in athletics, a short Achilles tendon, direct trauma (injury) to the tendon, training errors and heel bone deformity. There is significant evidence that people with feet that role in excessively (over-pronate) are at greater risk for developing Achilles tendinitis. The increased pronation puts additional stress on the tendon, therefore, placing it at greater risk for injury.
Symptoms
Signs and symptoms of Achilles Tendinitis generally include pain and stiffness along your achilles tendon, especially in the morning. Pain in the back of your heel that gets worse with activity. Severe pain the day after exercising. Swelling that gets worse with activity. If you feel a pop in the back of your heel or bottom of you calf, you may have ruptured or torn you achilles tendon.
Diagnosis
When diagnosing Achilles tendinitis, a doctor will ask the patient a few questions about their symptoms and then perform a physical examination. To perform a physical exam on the Achilles tendon, the doctor will lightly touch around the back of the ankle and tendon to locate the source of the pain or inflammation. They will also test the foot and ankle to see if their range of motion and flexibility has been impaired. The doctor might also order an imaging test to be done on the tendon. This will aid in the elimination of other possible causes of pain and swelling, and may help the doctor assess the level of damage (if any) that has been done to the tendon. Types of imaging tests that could be used for diagnosing Achilles tendinitis are MRI (Magnetic resonance imaging), X-ray, Ultrasound.
Nonsurgical Treatment
Treatment for Achilles tendonitis, depends on the severity of the injury. If heel pain, tenderness, swelling, or discomfort in the back of the lower leg occurs, physical activity that produces the symptoms should be discontinued. If the problem returns or persists, a medical professional should be consulted. If pain develops even with proper stretching and training techniques, the patient should consult a podiatrist to check for hyperpronation and adequate arch support. The addition of an orthotic may be enough to maintain good arch and foot alignment and eliminate pain. If damage to the tendon is minor, the injury may respond to a simple course of treatment known as RICE (rest, ice, compression, elevation). Patients are advised to rest the tendon by keeping off their feet as much as possible, apply ice packs for 20 minutes at a time every hour for a day or two to reduce swelling, compress the ankle and foot with a firmly (not tightly) wrapped elastic bandage and elevate the foot whenever possible to minimize swelling. A nonsteroidal anti-inflammatory drug (NSAID) such as ibuprofen may be used to reduce pain, swelling, and inflammation.

Surgical Treatment
If several months of more-conservative treatments don't work or if the tendon has torn, your doctor may suggest surgery to repair your Achilles tendon.
Prevention
Suggestions to reduce your risk of Achilles tendonitis include, incorporate stretching into your warm-up and cool-down routines, maintain an adequate level of fitness for your sport, avoid dramatic increases in sports training, if you experience pain in your Achilles tendon, rest the area. Trying to ?work through? the pain will only make your injury worse, wear good quality supportive shoes appropriate to your sport. If there is foot deformity or flattening, obtain orthoses, avoid wearing high heels on a regular basis. Maintaining your foot in a ?tiptoe? position shortens your calf muscles and reduces the flexibility of your Achilles tendon. An inflexible Achilles tendon is more susceptible to injury, maintain a normal healthy weight.
What Are The Presenting Symptoms Of Hallux Valgus?
Most bunions can be treated without surgery. But when nonsurgical treatments are not enough, surgery can relieve your pain, correct any related foot deformity, and help you resume your normal activities. An orthopaedic surgeon can help you decide if surgery is the best option for you. Whether you've just begun exploring treatment for bunions or have already decided with your orthopaedic surgeon to have surgery, this booklet will help you understand more about this valuable procedure. Failure to obtain pain relief from nonsteroidal anti-inflammatory drugs. Their effectiveness in controlling toe pain varies greatly from person to person. Not only are the angles that form the bunion important, but the actual condition of the joint itself is also very important. If the cartilage making up the joint is too far eroded then even a procedure that creates perfect alignment of the joint is still going to be problematic for the patient. It is at this point that the surgeon has to decide to either remodel the joint or replace the joint with an implant or artificial joint. Unfortunately, the only real way to know the actual condition of the joint is to visually inspect it, once the foot is open. A study by the American Orthopaedic Foot and Ankle Society found that 88 percent of women in the U.S. wear shoes that are too small and 55 percent have bunions. Not surprisingly, bunions are nine times more common in women than men. Some shoes can be modified by stretching the areas that put pressure on your toes. Splints to reposition the big toe and orthotics (special shoe inserts shaped to your feet) also may relieve pain. For bunions caused by arthritis, medications can be prescribed to reduce pain and swelling. Dr. Prateek Gupta M.S., M.ch-orth(Livepool),FICS(USA), D.Orth.(London), F.R.C.S - Orth(London), Consultant Orthopedics & Sports Surgeon. Sir Gangaram Hospital, New Delhi, India. When the above non-surgical treatment options have not worked, the health care provider will suggest undergoing a bunion surgery to correct the dislocation. The surgery can be performed by an orthopedic surgeon, who will loosen the tight tissues and shorten the long ones, so as to repair the tendons and ligaments present around the toe. Severe bunions can be corrected with the use of wires, plates and screws. There are different types of surgical procedures and the best procedure for you will be told to you by your surgeon. Bunion surgeries cannot be guaranteed for a total recovery. Often calluses and corns are developed as post operative complications. Orthotics, custom orthopedic foot supports, can help with mild hammer toes and bunions. They aren't a cure, but orthotics can make certain types of shoes more comfortable. Orthotics may slow down or perhaps prevent the progression of bunions and hammer toes. However, once the hammer toes and bunions become too large or severe an orthotic becomes just another thing occupying space in a crowded shoe. How does the nursery rhyme go? There was an old lady living in a shoe with so many hammer toes and bunions she didn't know what to do. Treat the pain with pain relievers, use pads to cover the bunions, buy shoe inserts, or surgery may be an effective option for you. Avoid wearing high heels and wear roomy shoes for comfort. Corn and calluses are dead thickened skin that is caused by friction. The thick skin forms to protect the sensitive skin on the foot. These will go away when you reduce the friction of the irritated area. Moleskin pads can eliminate corns and calluses can be trimmed or surgically removed. Other related procedures that may be used to help diagnose foot disorders include X-rays of the bone and foot. Please see these procedures for additional information. A bunion is an enlargement of bone or tissue around the metatarsophalangeal (MTP) joint of the great toe. It's often caused by patients wearing shoes that are too narrow around the toe box and can cause pain and deformity of the toes. If the patient's great toe is not overlapping or impinging upon the second toe, but he still has an obvious bunion, take a look at 727.1; this code specifically says 'bunion' and the ICD-9 definition is "enlarged first metatarsal head due to inflamed bursa; results in laterally displaced great toe." There is some controversy in the medical community about the benefit of physical therapy after surgery. I do not send all my patients for physical therapy; in fact in many cases I will just give them instructions in exercises and other things they can do at home to facilitate their healing (and only hope they actually follow my instructions). If after reading this page you are still "up in the air" as to what you should do about your bunion, may I suggest you visit the following web site for a personal account of one person's experience with a variety of non-surgical bunion treatments The bunion experiment TAILORS BUNION
Orthotics, custom orthopedic foot supports, can help with mild hammer toes and bunions. They aren't a cure, but orthotics can make certain types of shoes more comfortable. Orthotics may slow down or perhaps prevent the progression of bunions and hammer toes. However, once the hammer toes and bunions become too large or severe an orthotic becomes just another thing occupying space in a crowded shoe. How does the nursery rhyme go? There was an old lady living in a shoe with so many hammer toes and bunions she didn't know what to do. Treat the pain with pain relievers, use pads to cover the bunions, buy shoe inserts, or surgery may be an effective option for you. Avoid wearing high heels and wear roomy shoes for comfort. Corn and calluses are dead thickened skin that is caused by friction. The thick skin forms to protect the sensitive skin on the foot. These will go away when you reduce the friction of the irritated area. Moleskin pads can eliminate corns and calluses can be trimmed or surgically removed. Other related procedures that may be used to help diagnose foot disorders include X-rays of the bone and foot. Please see these procedures for additional information. A bunion is an enlargement of bone or tissue around the metatarsophalangeal (MTP) joint of the great toe. It's often caused by patients wearing shoes that are too narrow around the toe box and can cause pain and deformity of the toes. If the patient's great toe is not overlapping or impinging upon the second toe, but he still has an obvious bunion, take a look at 727.1; this code specifically says 'bunion' and the ICD-9 definition is "enlarged first metatarsal head due to inflamed bursa; results in laterally displaced great toe." There is some controversy in the medical community about the benefit of physical therapy after surgery. I do not send all my patients for physical therapy; in fact in many cases I will just give them instructions in exercises and other things they can do at home to facilitate their healing (and only hope they actually follow my instructions). If after reading this page you are still "up in the air" as to what you should do about your bunion, may I suggest you visit the following web site for a personal account of one person's experience with a variety of non-surgical bunion treatments The bunion experiment TAILORS BUNION A bunion is caused by an abnormality in the position of the bones in the foot and big toe. Instead of being in line, meeting flatly end-to-end, the bone along the inside of the foot (the first metatarsal) and the first bone of the big toe ( hallux ) meet at an angle ( valgus deformity). The only way that they can be corrected is by surgery. In the past, surgical operations had meant being off one's feet and in plaster for up to three months. Called osteotomy, this conventional surgery involves cutting out a piece of bone and repositioning the two ends to try and straighten the toe.
A bunion is caused by an abnormality in the position of the bones in the foot and big toe. Instead of being in line, meeting flatly end-to-end, the bone along the inside of the foot (the first metatarsal) and the first bone of the big toe ( hallux ) meet at an angle ( valgus deformity). The only way that they can be corrected is by surgery. In the past, surgical operations had meant being off one's feet and in plaster for up to three months. Called osteotomy, this conventional surgery involves cutting out a piece of bone and repositioning the two ends to try and straighten the toe.
Foot Pain Causes And Treatments
Excellent for medical ailments– Crocs are perfect for people with foot conditions and deformities that are aggravated by shoes with toe boxes that are too tight. Crocs provide a wide and roomy toe box, with lots of room for toes to spread out and lie flat.Crocs also offer a supportive heel cup that makes them an excellent choice for people that have swollen feet (plantar fascilitis). The contoured foot bed is designed to promote stability and reduce excess pronation. Cold hand treatment and prevention includes wearing gloves and socks even when you are indoors. You can try the following tips for cold hand treatment and prevent this condition. With acute ankle sprains representing nearly 20 percent of the sports-related injuries suffered yearly in the United States, it is important for coaches and others associated with athletics to know the proper procedure for taping an ankle. In addition to taping injured ankles, most athletic trainers suggest ankle taping as an injury-prevention measure-especially for those athletes who have suffered previous ankle sprains. Taping an ankle is not a complicated procedure, but it does require a person to follow step-by-step guidelines to provide effective support of the injured ankle. 10.if have a history of athletes foot ppl can dust antifungal powder on feet to prevent getting it again Wearing high-heeled shoes can also stretch the ligament beyond the tolerable limits and cause inflammation. Those suffering from plantar fasciitis are also at an increased risk of developing heel spurs. Heel spurs also known as osteophytes are abnormal bony outgrowths that may develop along the edges of the heel bone. Heel spurs form when the plantar fascia starts pulling at the heel bone or gets torn due to excessive stress. footwear along with tips on buying the right type of shoes that may help to prevent plantar fasciitis and heel spurs. Can Poorly-fitted Shoes Cause Heel Spurs and Plantar Fasciitis? Plantar fasciitis is associated with the inflammation of plantar fascia. While a sprained ankle usually heals quickly and is not a disabling injury, too many sprains due to athletics or other physical activities can weaken the overall strength of the ankle over time. Wrapping a sprain will decrease discomfort associated with a sprain and also add support to prevent this gradual weakening. Taping an ankle before strenuous activity can also be used to prevent sprains and injury. The researchers set up a prospective, experimental, randomized, double-blinded, and controlled clinical trial, where patients were treated either with steroids or with Botox for their painful feet. Both groups were shown the same series of physical exercises to help their recovery. Varicose veins – Twisted, enlarged veins near the surface of the skin. They most commonly develop in the legs and ankles. Varicose veins develop when you have faulty valves in your veins and weakened vein walls. Normally, the one-way valves in these veins keep the blood flowing efficiently against gravity up toward the heart. When these valves do not function properly, blood pools, pressure builds up, and the veins become weakened, enlarged, and twisted. This is called venous insufficiency. This is where Easy Feet comes in. Easy Feet is a fantastic new product that allows you to clean and massage your feet without having to bend over to do it. We have recommended many male consumers to try on a female size FiveFingers and have had great success. The only difference between a male and female FiveFingers is that, male "lasts" are slightly wider and longer than the female models. If your foot is smaller than the smallest male size, certainly try on a female size based on your measurement in inches -you may have much better luck! Alternately, if you are a woman and your foot is bigger than the largest female size, we encourage you to try one of our Men's models based on your foot measurement in inches. Â
While a sprained ankle usually heals quickly and is not a disabling injury, too many sprains due to athletics or other physical activities can weaken the overall strength of the ankle over time. Wrapping a sprain will decrease discomfort associated with a sprain and also add support to prevent this gradual weakening. Taping an ankle before strenuous activity can also be used to prevent sprains and injury. The researchers set up a prospective, experimental, randomized, double-blinded, and controlled clinical trial, where patients were treated either with steroids or with Botox for their painful feet. Both groups were shown the same series of physical exercises to help their recovery. Varicose veins – Twisted, enlarged veins near the surface of the skin. They most commonly develop in the legs and ankles. Varicose veins develop when you have faulty valves in your veins and weakened vein walls. Normally, the one-way valves in these veins keep the blood flowing efficiently against gravity up toward the heart. When these valves do not function properly, blood pools, pressure builds up, and the veins become weakened, enlarged, and twisted. This is called venous insufficiency. This is where Easy Feet comes in. Easy Feet is a fantastic new product that allows you to clean and massage your feet without having to bend over to do it. We have recommended many male consumers to try on a female size FiveFingers and have had great success. The only difference between a male and female FiveFingers is that, male "lasts" are slightly wider and longer than the female models. If your foot is smaller than the smallest male size, certainly try on a female size based on your measurement in inches -you may have much better luck! Alternately, if you are a woman and your foot is bigger than the largest female size, we encourage you to try one of our Men's models based on your foot measurement in inches. Â